Anand Kumar: Premature Alzheimer’s diagnosis using pseudoscience is dangerous
When I turned 60, my primary-care physician said something profound: “There is no reason for someone to wake up in this day and age and find that they have advanced colon cancer.” It was a nudge in the right direction.
Early detection and early intervention have been medicine’s mantra for the past several decades. Medical societies recommend colonoscopy and mammograms, for example, to individuals who are at minimal risk. This is based on the presumption that the biological processes that lead to the disease begin years, if not decades, before the disease becomes manifest. Detecting the disease in its “preclinical” state will result in early treatment that will prolong and improve the quality of life.
In the case of Alzheimer’s disease, some of the biological processes responsible for the condition are also presumed to begin two to three decades before the early symptoms of the disease first appear.
Despite the multiple risk factors involved, two proteins found in the brains of Alzheimer’s disease patients — beta amyloid and tau — have dominated the interest of researchers, federal funding and pharmaceutical research support. Academic researchers, pharmaceutical companies, advocacy groups and branches of federal government have formed a team that argues for a central role for these proteins beyond what the objective scientific evidence currently supports.
A recent conference in Amsterdam, dominated by researchers with strong ties to the pharmaceutical industry, recommended updated criteria for the diagnosis of Alzheimer’s disease. Should these recommendations be actualized, individuals with no cognitive or behavioral symptoms will be diagnosed as having Stage 1 of Alzheimer’s disease if they test positive for amyloid. Cognitive abnormalities that can be documented will be required for a diagnosis only in the more advanced stages of the disease. If these criteria are more broadly adopted, many cognitively and behaviorally normal individuals in their 40s and 50s will be diagnosed as having the disease based on an amyloid test alone. This sets the stage for placing them on expensive medications with modest therapeutic effects but serious side effects for a disease that many do not have and may never get.
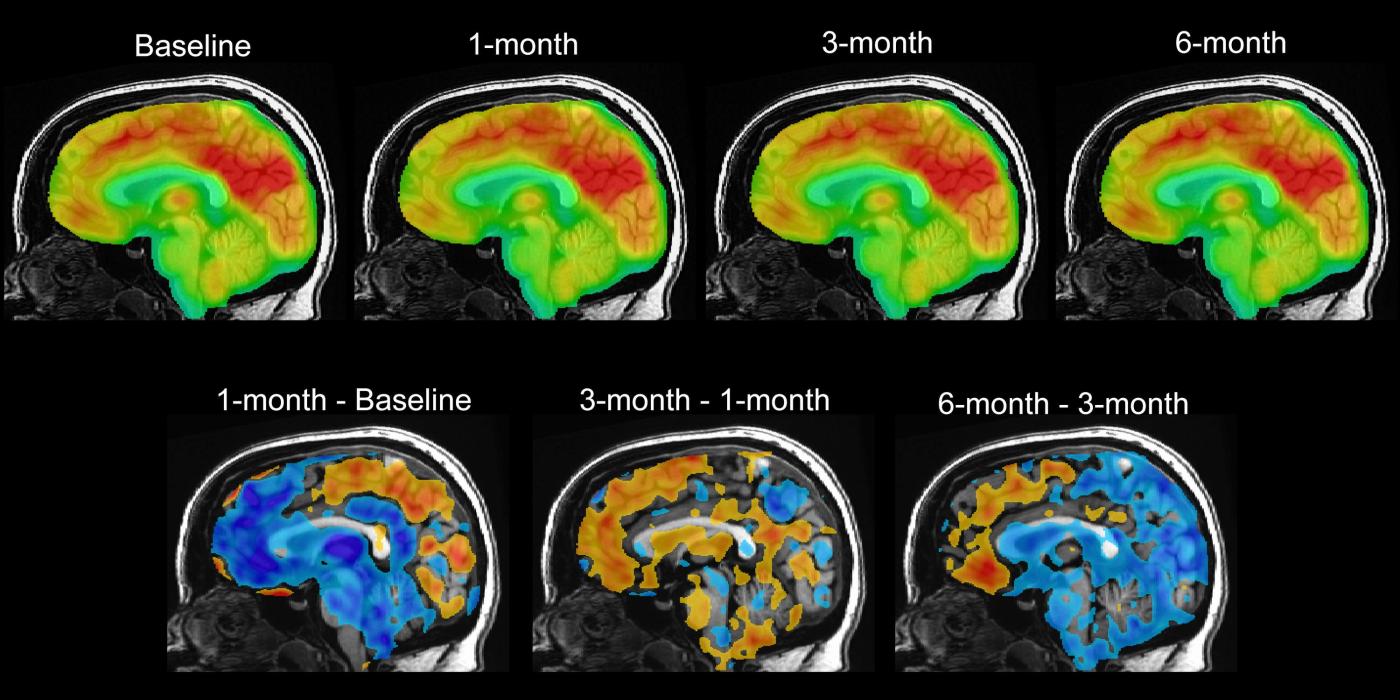
Amyloid and tau are considered biomarkers for the disease — laboratory-based measures that are useful in diagnosing the disease, monitoring its progression and studying the impact of treatment. Levels of amyloid and tau can be detected using specialized brain scans; studies of cerebrospinal fluid, which cover the brain and spinal cord; and, more recently, blood tests.
But here is the critical caveat: Not all patients who have elevated levels of amyloid and tau will develop Alzheimer’s disease, and not all patients with a clinical picture consistent with the disease have elevated levels of amyloid and tau.
In other words, these tests are not definitive by themselves and need strong clinical corroboration, and it is the totality of the picture — clinical presentation plus relevant testing — that is needed to confirm the diagnosis.
There is evidence to suggest that a high proportion of patients in their 50s, 60s and 70s will test positive but will never develop the disease. The amyloid tests are not comparable to colonoscopies and mammograms in which a pathological report is used to corroborate imaging abnormalities before any intervention is made.
Further, in the case of Alzheimer’s, amyloid and tau serve as therapeutic targets for drug development. Over the past few decades, such efforts have disproportionately focused on compounds that reduce the levels of both proteins in the brain. The evidence that amyloid-lowering drugs have a meaningful impact in Alzheimer’s disease is modest, at best.
There are good and bad medical practices. This one is horrifying. The combination of an amyloid test, possibly just a blood test, and research demonstrating that the disease starts much earlier than the clinical presentation has shifted the discussion in favor of premature diagnosis, poorly applied public health principles and the potential use of expensive drugs with serious side effects in young normal adults. Labeling healthy individuals who have an abnormal blood test as having Alzheimer’s disease is scientifically unsound and ethically suspect, especially considering that many of them will never develop the disease. Neuroprotective agents should unambiguously protect neurons and be given only to individuals whose neurons need protection.
What society needs are biomarker-based tests that are validated and standardized using objective population health concepts and guidelines in order to determine how specific and sensitive they really are in individuals without cognitive signs and symptoms. This step is critical to preclude over-interpretation of laboratory test results in broader populations.
We also need drugs that are demonstrably effective on meaningful, real-world outcomes while remaining affordable and free of life-threatening side effects. Simply put, the risk and cost-benefit analyses need to be reasonable and acceptable.
Academic researchers, advocacy groups and relevant branches of the federal government have a moral and ethical responsibility in this regard. After all, they are the entities funding and advancing this agenda. The scientific bar should be very high before we diagnose healthy individuals with Alzheimer’s disease. The implications of this diagnosis must not be trivialized.
Inappropriately diagnosing and treating typical Americans with expensive drugs that promise to “prevent” Alzheimer’s disease does not constitute scientific progress. It is a slippery slope that will get more slippery over time.
The saying primum non nocere, or “first do no harm” — attributed to the ancient Greek doctor Hippocrates — is one of the promises that graduating medical students make as they begin their journey. Let us never forget that promise. Let us work to gain the public trust.
Dr. Anand Kumar is a professor and head of the department of psychiatry at the University of Illinois at Chicago and past president of the American Association for Geriatric Psychiatry. He wrote this column for the Chicago Tribune.
Related Articles
Daniel DePetris: A belligerent China is bringing out East Asia’s resolve
Farah Stockman: Is this the Silicon Valley of Latin America?
Bret Stephens: The appalling tactics of the ‘Free Palestine’ movement
Tyler Cowen: Indiana can’t make universities more conservative with a law
Zeynep Tufekci: You don’t need to freak out about Boeing planes (but Boeing does)


